Abstract
Introduction: While both race/ ethnicity & socioeconomic status (SES) impact care delivery for allograft candidates & recipients, the associations between ancestry & SES, & their interaction with donor type are not fully established. We hypothesized that low SES disproportionately impacts non-European (non-EURO) recipients of HLA-disparate grafts (cord blood, haploidentical, or 4-7/8 unrelated donor [mmURD]).
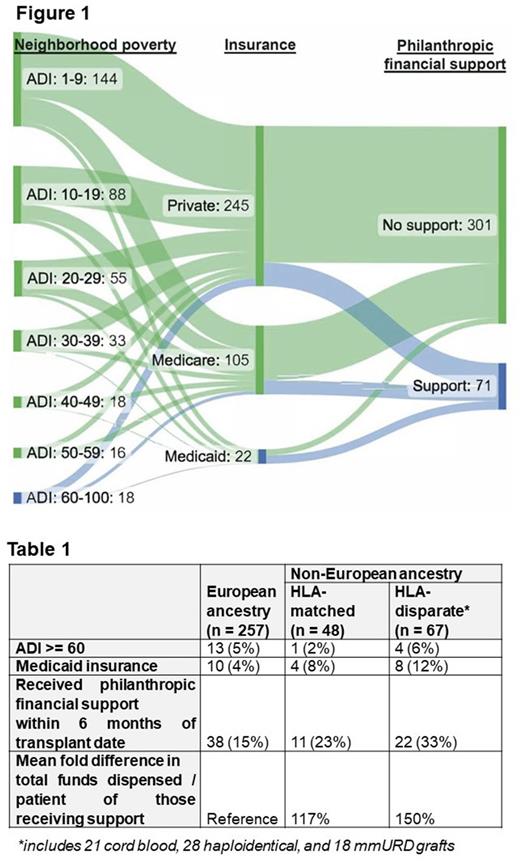
Methods: We examined surrogates of SES in consecutive adults undergoing allograft 3/2020-2/2022 stratified by recipient ancestry & donor type. A 3/2020 analysis commencement was selected as Social Work (SW) philanthropic financial support for vulnerable patients increased at the onset of the COVID-19 pandemic. As household income was not collected, surrogates of low SES were defined as: 1) an area deprivation index (ADI) national percentile ≥ 60; 2) Medicaid as the primary insurance at BMT referral; &/ or 3) received SW philanthropic financial support to cover cost-of-living expenses within 6 months of transplant. We also assessed mean fold differences in the funding amount/ patient receiving philanthropic support.
Results: Of 372 patients (pts, median 62 years, range 19-81; 73% myeloid malignancy), 257 (69%) had European (EURO) and 115 (31%) non-EURO ancestry (including 31 White Hispanic, 40 African, 34 Asian, 4 Middle Eastern, and 6 mixed non-EURO pts). 53 (14%) received matched sibling donor, 191 (51%) 8/8 unrelated donor, 38 (10%) cord blood, 47 (13%) haploidentical, and 43 (12%) mmURD transplants. More than half (67/115, 58%) of non-EURO ancestry pts received an HLA-disparate graft compared to 24% (61/257) of EURO pts (p < 0.001). Median ADI was 14 (range 1-100). Eighteen (5%) patients had low SES by ADI ≥ 60; 22 (6%) by Medicaid insurance; and 71 (19%) by receipt of financial support.
A higher proportion of pts received financial support if they had Medicaid (13/22, 59%) compared to Medicare/ private insurance (58/350, 17%), p < 0.001, or if their ADI was ≥ 60 (7/18, 38%) compared to < 60 (64/354, 18%), p = 0.028. Conversely, only one pt with ADI ≥ 60 had Medicaid. Notably, the 3 SES classifications resulted in different pts being classified as low SES (Figure 1). Only 20 pts had low SES by two of these measures, & only 1 by all three.
When analyzing by ancestry, compared to EUROs, non-EUROs had a similar ADI distribution but over double the proportion on Medicaid (12/115, 10% vs 10/257, 4%, p = 0.013). Non-EUROs also had almost twice the proportion receiving financial support (33/115, 29% vs 38/257, 15%, p = 0.002), & those who did were granted a mean of 40% more funds relative to EUROs. African ancestry pts had the highest proportions on Medicaid (5/40, 12.5%) & receiving financial support (17/40, 42.5%), with the highest mean fold increase in funds (58% more) relative to EUROs.
When stratifying by both ancestry & graft source, because very few EURO HLA-disparate graft recipients had low SES, all EURO ancestry pts were combined. Relative to EUROs, non-EUROs who received HLA-disparate grafts (n = 67 including 15 White Hispanic, 31 African, 20 Asian, & 1 mixed non-EURO pts) had triple the proportion on Medicaid (8/67, 12% vs 10/257, 4%, p = 0.015) with more than double receiving financial support (22/67, 33% vs 38/257, 15%, p = 0.001). Also, those who received support were granted a mean of 50% more funds relative to EUROs (Table 1). By contrast, differences between EUROs & non-EURO HLA-matched graft recipients were not significant. African ancestry pts who received HLA-disparate grafts had the highest proportions on Medicaid (5/31, 16%) & receiving financial support (14/31, 45%) with the highest mean fold increase in funds (75% more) relative to EURO pts.
Conclusions: We demonstrate an intersectionality between ancestry & SES, & an association with donor type, with the most vulnerable patients (non-EUROs with low SES, especially African ancestry pts) receiving the most complex (ie HLA-disparate) transplants. Successful extension of transplant access to minority pts will be contingent on addressing this financial hardship. Moreover, as the different SES classification systems result in different assignment of SES, interventions to advance equity will require better SES classifications or detailed recording of household income. Access to expensive post-transplant medications may be another surrogate of low SES & analysis of this is underway at our Center.
Disclosures
Shaffer:Gamida Cell: Consultancy; Miltenyi Biotec: Research Funding; Hansa Biopharma: Consultancy. Shah:Beyond Spring: Research Funding; Janssen: Research Funding; Amgen: Research Funding. Barker:Gamida Cell: Consultancy; New York Blood Center: Consultancy; Merck: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal